Playback speed:
The type of food we eat will affect our health and quality of life. While there is no special diet required for persons living with dementia, the condition may bring about challenges to proper nutrition, hydration, and weight maintenance. Here are a few ways to ensure that your loved one has a well-balanced and nutritious diet, drinks sufficient amounts of liquid, and maintains physical and mental well-being.
Why is Proper Nutrition & Hydration Especially Important for Persons Living with Dementia?
The nutritional and hydration needs of persons living with dementia will be similar to other people of their age. People who are undernourished tend to get sick more often and recover from illness and injury more slowly. However, those who experience increased physical activity from restless behaviours (such as pacing up and down, wandering and fidgeting), may need a higher amount of nutrients to try to minimize weight loss.
For most persons living with dementia, maintaining good nutrition may be a challenge. Some of the changes they may experience include a loss of appetite, forgetting to eat and drink, forgetting how to chew or swallow, or developing an insatiable appetite.1
People in the later stages of dementia may lose a considerable amount of weight. Learn about strategies to help promote oral intake and create a positive eating environment here. If there is persistent weight loss or poor appetite despite these strategies, it is recommended to seek advice from a dietitian.
Eating Well for Healthy Ageing
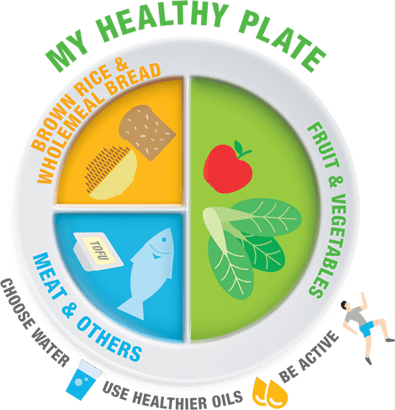
Eating a well-balanced nutritious diet is important for overall health. My Healthy Plate shows the portions required for a balanced and healthy diet, which is a guideline for one to aim for.
¼ Plate of Wholegrains

Wholegrains provide us with energy, fibre, vitamins (e.g. vitamin B and vitamin E) and minerals (e.g. zinc, magnesium). They are rich in nutrients as they are not overly processed, with their original form being kept. Eating more wholegrains have been shown to lower one’s risk of developing chronic diseases such as diabetes, heart diseases and certain cancers.
Wholegrains include brown rice, wholegrain bread and oatmeal. Wholegrains can also be used to make products such as brown rice vermicelli, chapati from wholemeal flour and wholegrain breakfast cereals.
It is recommended to consume at least 2-3 servings of carbohydrates/wholegrains per day
1 serving of protein equals to: | |
1 palm size of lean meat/poultry/fish | 2 glasses of low-fat milk |
4 slices of low-fat cheese | ¾ cup of cooked beans/peas/lentils (120g) |
4 pieces of tempeh (120g) | ¾ block of tau kwa (150g) |

Incorporating a variety of wholegrains will help to ensure one gets more nutrients and makes mealtime more interesting. Do keep a look out for “Higher in Wholegrains” Healthier Choice Symbol during grocery shopping.
Meeting the above protein requirements per day will help to ensure that one gets sufficient amounts of iron and vitamin B12 daily. Iron and vitamin B12 help in the formation of haemoglobin in our red blood cells, which are needed to carry oxygen to all parts of our body. There are two types of iron in foods. Haem iron comes from animal sources (such as meat, poultry, fish) and non-haem iron come from eggs and plant sources (such as beans, lentils, peas), nuts, fruits and vegetables. Our body absorbs haem iron better than non-haem iron. Eating foods rich in vitamin C (e.g. oranges, lemons, tomatoes, cabbage) together with foods containing non-haem iron, and drinking coffee/tea away from meals are some ways to help to increase iron absorption. Sources of vitamin B12 include meat, fish egg, yoghurt, fortified soymilk and fortified cereal.
Dairy products (low fat milk/cheese/yoghurt), high calcium soy milk, tofu and canned low sodium sardines are both good sources of protein and calcium. Calcium helps to strengthen our bones and teeth and reduces the risk of osteoporosis. Drinking 2 cups of high calcium low-fat milk or high calcium soy milk will allow one to meet their daily calcium requirements of 1000mg per day. Vitamin D helps our body to better absorb calcium into our body. Food sources of vitamin D include oily fish (e.g. salmon, mackerel, cod), eggs, margarine, fortified cereals, fortified dairy (milk, cheese, yoghurt) and fortified soy milk. Meeting above protein and calcium requirements will generally mean that one is meeting recommended amounts of vitamin D per day.
½ Plate of Vegetables and Fruits

Similar to wholegrains, vegetables and fruits are rich in fibre. They are also rich in vitamins, minerals, phytochemicals and antioxidants. Consumption of adequate fibre daily helps protect one against chronic diseases such as heart diseases, stroke and certain cancers. Fibre helps to regulate our bowel movement, control blood sugar and cholesterol levels, and manage weight gain.
It is recommended for women to take 20g of fibre per day and men to take 26g of fibre per day. This equates to 2 servings of vegetables and 2 servings of fruits per day. Starchy or root vegetables like corn, sweet potato and potato do not count towards the 2 serves of vegetables per day.
1 serving of fruit equals to: | |
1 small apple, orange, pear or mango (130g) | 1 wedge of papaya, pineapple or watermelon (130g) |
1 medium banana | 10 grapes or longans |
1 serving of vegetable equals to: | |
¼ round plate of cooked vegetables | 150g of raw leafy vegetables |
¾ cup of cooked leafy vegetables (100g) | 100g of raw non-leafy vegetables |
¾ cup of non-leafy vegetables (100g) |
|
Overall, it is recommended to:
- Enjoy a wide variety of nutritious foods across and within food groups
- Eat at least 3 meals a day
- Eat 2 servings of fruits and 2 servings of vegetables a day
- Eat a diet low in saturated fats and salt
- Include foods containing calcium, vitamin D, iron and vitamin B12
- Use added sugars in moderation
Drinking Enough Fluids
Persons living with dementia who are older may be more susceptible to dehydration due to reasons such as a blunted sense of thirst, poor memory, immobility or medications interfering with their thirst mechanism.2 Low hydration levels are associated with incidences of acute confusion/delirium, urinary tract infections, constipation and delayed wound healing.3
It is recommended to aim for 6-8 glasses of water per day.
Tips to increase fluid intake include:
- Frequent encouragement of small amounts of fluids throughout the day
- Keep a cup/bottle of water within reach of the elderly
- If the senior is not keen on drinking plain fluids, other sources of fluids such as soup, juices, milk, honey water, barley water can be encouraged
Preservation of Cognitive Function
There is currently a move in research to consider the evidence for whole diets (particularly those which are plant-based, rich in good fats), rather than individual nutrients, to help with the prevention of cognitive and functional decline.4 This could probably be due to the synergistic beneficial effects of various nutrients in a diet.5
Research suggests that healthy dietary patterns with an emphasis on higher consumption of vegetables, fruits, wholegrains and healthy fats, while minimising red meat, refined sugars and processed foods intake may work as a preventative measure to cognitive decline by reducing cardiovascular risks.4
Some examples include the Mediterranean Diet, Dietary Approaches to Stop Hypertension (DASH) Diet, Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) Diet and NU-AGE Diet.
Understanding Dementia: Part 7
Source: Agency for Integrated Care
Today, there has been no clear and consistent information on dietary factors that may increase or decrease the risk for the onset of dementia. However, adopting a Mediterranean diet may lower the risk of cognitive decline and dementia. This means eating higher proportions of grains, fruits, fish and vegetables.
These dietary patterns share similar recommendations with My Healthy Plate from the Health Promotion Board (Singapore), though with additional advice for specific food groups and portion sizes. In common, these dietary patterns recommend:
- Selecting wholegrains (aim for at least 2 serves of wholegrains per day)
- Choose lean meat and oily fish (aim for at least 1 serving of oily fish such as sardine, mackerel, and salmon per week)
- Aim for at least 2-3 serves of vegetables per day
- Aim for at least 2 servings of fruits per day, including 2 serves of berries per week
- Incorporate healthy oils (e.g. olive oil)
However, current research has not yet been able to determine how long the exposure to these diets must be or during which ages is it more effective.4 Hence, individuals should be encouraged to follow the above recommendations if they are nutritionally well, as a preventative measure to cognitive decline. There should also be focus on meeting caloric and protein requirements for individuals who are undernourished as poor nutrition can lead to a myriad of health issues.
Additional Resources
Nutrition and Dementia
Source: Alzheimer’s Disease International
This report investigates how a healthy diet and the right nutrition can improve the lives of persons living with dementia. The publication features:
- Dietary factors across the life course that might increase or decrease the risk of onset of dementia in later life;
- Relationship between dietary nutrients and dementia prevention;
- Recommendations on the actions to take in order to improve the nutrition of persons living with dementia; and
- The need for more research on nutrition and dementia.
Eating Well with Dementia
Source: Alzheimer’s Society of Ireland
- Provides caregivers with information on:
- Understanding how dementia can affect a person’s appetite and experience with food;
- Meeting the nutritional needs of a person with dementia;
- Encouraging a person with dementia to enjoy and be involved in meal preparation and mealtimes; and
- Dealing with weight loss, weight gain and other issues that can emerge.
Eating and Living With Dignity
Source: Ministry of Health of Israel
This guide for care professionals and family caregivers provides information, tips, and recommendations addressing the following in persons with dementia, such as:
- Difficulties with eating and choosing food;
- Constipation problems;
- Changes in eating and swallowing as dementia progresses; and
- Maintaining health nutrition.
AUTHOR BIO

Clarissa Tai, Senior Dietitian
After graduating from the University of Queensland with a Master in Dietetics degree, Clarissa has been working as a dietitian at Tan Tock Seng Hospital since 2019. Her interest lies in working with the geriatric population, to help improve their health, quality of life and awareness of nutrition related issues.
Tell us how we can improve?
- Volkert D, Chourdakis M, Faxen-Irving G, et al. ESPEN guidelines on nutrition in dementia. Clinical Nutrition [Internet]. 2015 [cited 2022 Aug];34(6):1052-73. Available from https://nutritotal.com.br/pro/wp-content/uploads/sites/3/2016/03/ESPEN_demencia.pdf
- El-Sharkawy AM, Watson P, Neal KR, et al. Hydration and outcome in older patients admitted to hospital (The HOOP prospective cohort study). Age Ageing [Internet]. 2015 [cited 2022 Sept];44(6):943-947. Available from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4621229/
- Bruno C, Collier A, Holyday M, Lambert K. Interventions to improve hydration in older adults: A systematic review and meta-analysis. Nutrients [Internet]. 2021 [cited 2022 Sept];13(10):3640. Available from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4621229 DOI: 10.1093/ageing/afv119
- Lavingston G, Huntley J, Sommerlad A, et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. The Lancet [Internet]. 2020 [cited 2022 Aug];396(10248):413-446. Available from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7392084/
- Scarmeas N, Anastasiou CA, Yannakoulia M. Nutrition and prevention of cognitive decline. The Lancet Neurology [Internet]. 2018 [cited 2022 Aug];17(11):1006-15. Available from http://old.school.med.uoa.gr/uploads/media/LancetNeurology2018.pdf




