Vascular dementia is one of the most common types of dementia in Singapore. In fact, 45.5% or almost half of those with dementia in Singapore have this condition. 1 Read on to find out more about what it is, its symptoms and risk factors, and how to reduce the risk of developing this type of dementia.
What is Vascular Dementia?
Vascular dementia is a type of dementia caused by blood-flow-related brain damage. The word ‘vascular’ refers to blood vessels.
How Common is Vascular Dementia?
Main Symptoms of Vascular Dementia
The symptoms of vascular dementia are similar to those experienced in other types of dementia. Typical symptoms include:
- Slow thought
- Difficulty with planning
- Trouble understanding
- Issues with concentration
- Mood and/or behaviour changes
- Memory and language issues
- Problems with movement and/or balance
The symptoms experienced depend on the specific brain areas that have been damaged. For example, if brain areas that are needed to understand language are damaged, a person with this kind of brain damage may have trouble understanding what they hear others saying, or what they read.
Read more about causes of vascular dementia in the sections below for more information of more specific groups of symptoms that can occur.
The speed of symptom development depends on the cause, type, and severity of the vascular dementia.
Symptoms of vascular dementia can develop slowly over time, which typically happens when the dementia is caused by chronic, slow-developing blood vessel damage.
On the other hand, symptoms can appear or worsen suddenly after a stroke: after both the first stroke and any subsequent strokes.
Symptoms of vascular dementia tend to be characterised more by speed of thought and problem-solving ability.
Some symptoms, like memory loss and language issues, tend to be more prominent in dementia caused by Alzheimer’s disease than in vascular dementia, although persons living with vascular dementia may experience them too.
The differences between the symptoms of vascular dementia and those of other kinds of dementia may be more obvious at the milder stages of dementia. As dementia progresses, the kinds of symptoms experienced may broaden in scope, and the differences between the symptoms of vascular dementia and other kinds of dementia may become less apparent.
A person can also develop mixed dementia, which happens when a person has more than one type of dementia. Most cases of mixed dementia happen with Alzheimer’s and vascular dementia since they are the two most common types of dementia. Persons with mixed dementia will show signs of both types of dementia, with one type of dementia often being predominant.
Causes
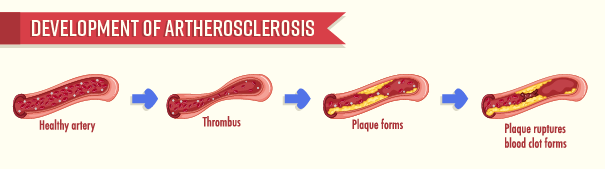
Blood carries nutrients and oxygen that our body’s cells need to work and be alive. When blood cannot reach certain brain tissues because of problems with blood flow, these tissues cannot receive the oxygen and nutrients they need and become damaged. If this lack of blood flow happens for too long, these tissues can die, causing irreversible damage.
Some of the more common vascular issues that can cause vascular dementia include:
The word ‘ischemia’ means ‘lack of blood flow’. An ischemic stroke is a blockage in a blood vessel in the brain. A single ischemic stroke or multiple strokes can prevent blood from reaching brain tissues.
The word ‘haemorrhage’ means bleeding. Haemorrhaging in the brain, or a haemorrhagic stroke, can happen in the brain’s blood vessels, and it is life-threatening when this happens. There are many possible causes of bleeding in the brain, including head trauma, high blood pressure that weakens blood vessels’ walls, and aneurysms (abnormal bulging in the walls of blood vessels).
Chronic blood vessel damage means damage to blood vessels that continues for a long time.
Damage to blood vessels, such as the narrowing of blood vessels, can, when it is severe, obstruct blood from flowing to brain tissues. Over time, this obstruction can develop into vascular dementia.
Types of Vascular Dementia
The symptoms of vascular dementia, and their order of development as dementia progresses, depend on the type of vascular dementia a person develops. The types of dementia are defined by different causes.
Below are the main types of vascular dementia:
- Subcortical vascular dementia happens when tiny blood vessels deep inside the brain become damaged.
- Most tissues damaged in this type of dementia happen in an area deep within the brain called the subcortex.
Stroke-related dementia happens when a stroke or multiple strokes happen in the brain. A stroke prevents blood from reaching brain tissues, leading to tissue death. The place where there is dead tissue due to low blood supply is called an ‘infarct’.
- Strategic-infarct dementia
-
- Strategic-infarct dementia happens when dementia is caused by one large stroke
- In this kind of dementia, there is a sudden and drastic change in thinking and behaviour, although with appropriate support, symptoms can be stabilised.
- Multi-infarct dementia
- Multi-infarct dementia happens when dementia is caused by a series of strokes which progressively damages brain tissue.
- Some strokes can be small and have minor symptoms. They can even happen without noticeable symptoms, in which case they are called ‘silent’ strokes.
- Smaller strokes are also called ministrokes or transient ischemic attacks (TIAs).
- Ministrokes can last for a few minutes each, and their more obvious symptoms can last for an hour to a day.
- As more strokes happen over time, symptoms of dementia can develop and worsen. The worsening of symptoms may be more noticeable immediately after each small stroke, after which the symptoms may tend to stabilise.
Stroke Syndromes
For both strategic-infarct and multi-infarct dementia, the parts of the brain that the stroke damages affects the syndrome (a group of symptoms) that a person experiences will differ. Knowing what stroke syndromes you or your loved one with vascular dementia may have can help you to better manage the symptoms of vascular dementia and get the appropriate support.
Many strokes will occur with hallmark stroke symptoms:
- Facial drooping of one side of the face
- Hemiparesis: weakness on one side of the body
- Numbness, usually on one side of the body
- Dysarthria: difficulty with speaking and/or slurred speech
- Dysphasia, or language impairment: an impaired ability to understand spoken and written language
- Confusion: trouble speaking and understanding speech
- Sight issues in either or both eyes
- Movement issues: trouble with walking; dizziness; difficulties with balance and coordination
- Severe headache without a known cause
These hallmark symptoms may not always happen in a stroke, or may happen with other syndromes depending on the type of stroke. The type of stroke itself depends on the area of the brain affected, including the side of the brain (right or left).
Some symptoms happen immediately when the stroke first happens, while others may develop after some time. In addition, some symptoms are long-lasting, while some symptoms involving the loss of abilities (for example. speech, sight) can sometimes be partially recovered.
More information about stroke syndromes can be found in the section Additional Information: Stroke Syndromes at the end of the article.
Treatment and Support
As vascular dementia is highly linked to vascular health issues, persons living with vascular dementia may be advised to take steps to improve their overall cardiovascular health, such as by improving their diet and level of physical activity.
Treatment and support after the diagnosis of vascular dementia may be done alongside treatment of health conditions that caused the dementia. For example, if a person has had a stroke that has led to the development of vascular dementia, this person may take medications for post-stroke treatment while undergoing rehabilitation therapies, such as physical therapy, speech therapy, and occupational therapy, to work on post-stroke issues.
Experiencing and adapting to vascular dementia are not easy for both the person experiencing the condition and their family and friends. It is, therefore, important to get support. Apart from the support from your community, support services are also available. For example, there are post-diagnostic support programmes that help to guide persons diagnosed with dementia and family caregivers through a period of time after diagnosis.
For more information on the support services available, contact a Community Outreach Team (CREST).
Risks
The risk of developing vascular dementia is closely linked to what affects one’s vascular health. Some risk factors for developing vascular dementia include:
- High blood pressure
- High blood cholesterol
- Diabetes
- Obesity
- Smoking
- Older age
How can I reduce my risk of developing vascular dementia?
In general, keeping one’s vascular system healthy and maintaining a healthy lifestyle helps to reduce the risk of developing vascular dementia.
Ways to keep one’s vascular system healthy:
- Moderate salt, sugar, and fat intake
- Eat sufficient fruits and vegetables
- Consume more wholegrain instead of refined carbohydrates like white rice or white bread
- Consume more protein-rich foods with healthy fats such as fish meat and beans over red meats
- It is recommended to have 150 minutes of moderate-intensity physical activity per week
- Do a good mix of aerobic exercise (exercise that speeds up your heart rate and breathing), strength-training exercise (exercise that maintains and builds muscle mass), stretching, and balance exercises
- In general, getting enough sleep lowers the risk for serious health problems
- Managing stress, especially long-term stress can improve heart health and mood, which in turn lowers the risk of developing vascular dementia
- Smoking damages blood vessels, which may make developing vascular dementia more likely
- Staying connected with others helps to regulate stress levels, which is good for vascular health
- Some ways you could keep connected could include: visiting Active Ageing Centres, volunteering in your community with others, organising occasions to eat together, or asking friends and/or family to do leisure activities together
Keep yourself engaged in activities that challenge yourself mentally. For example:
- Doing things that exercise your creativity (art activities, gardening, etc.)
- Learning new skills
- Playing games
- Having discussions with others
Watch this video by the Health Promotion Board to learn more about reducing the risk of developing vascular dementia.
Find out more about reducing the risk of developing dementia here.
How to get help:
If you or someone you know may have vascular dementia and need support or information, contact a Community Outreach Team (CREST) to find out more about getting support, or call Dementia Singapore’s helpline at 6377 0700.
Additional Information: Stroke Syndromes
A stroke syndrome is a group of symptoms that happens because of a stroke.
- Cerebellar strokes happen when blood vessel blockage or bleeding prevents blood flow to a part of the cerebellum.
- Cerebellar strokes are rare, and make up less than 10% of strokes.3
- Cerebellar stroke symptoms include:
- Dizziness and vertigo, with a feeling of falling to one side (occurs in 75% of cases of cerebellar stroke)4
- Nausea and vomiting (occurs in 50% of cases) 4
- Difficulty with walking
- Difficulties with coordination
- Tremors
- Headache
- Slurred speech
- Trouble with speech
- Double vision
- A pontine stroke happens when blood vessel blockage or bleeding prevents blood flow to a part of the brain stem called the pons.
- Pontine strokes are common, accounting for about 7% of strokes.5
- Pons and brain stem stroke symptoms may differ from the hallmark stroke symptoms, and may include:
- Dizziness, vertigo, and severe balance issues
- Double vision
- Slurred speech
- Swallowing difficulties
- Reduced alertness
- Motor and/or sensory impairment
- Hemiparesis: weakness and clumsiness in the face, arms, and legs on one side of the body
- A frontal lobe stroke happens when blood vessel blockage or bleeding prevents blood flow to the frontal lobes of the brain’s cerebral cortex.
- Frontal stroke symptoms include:
- Hemiparesis
- Speech issues
- Swallowing difficulties
- Incontinence
- Difficulties with spatial reasoning
- Changes in behaviour and personality
- Difficulties with executive functioning skills, such as reasoning, judgement, decision making, and problem solving
- A temporal lobe stroke happens when blood vessel blockage or bleeding prevents blood flow to the temporal lobes of the brain’s cerebral cortex.
- Temporal lobe stroke symptoms include:
- Speech issues
- Wernicke’s aphasia: a condition where a person is unable to understand the meaning of language spoken to them, or to produce meaningful language
- Hearing issues
- Hearing impairment may range from mild hearing loss to complete loss of hearing, which is rare
- Difficulties with processing sounds
- Auditory hallucinations
- Emotional changes such as fits of anger or aggression, or a lack of interest
- Difficulties with memory
- Speech issues
- A parietal lobe stroke happens when blood vessel blockage or bleeding prevents blood flow to the parietal lobes of the brain’s cerebral cortex.
- The symptoms of a parietal lobe stroke depend on whether the left or right parietal lobe is affected, and which side of the individual’s brain is more dominant for certain functions (e.g. language, mental calculations).
- In most cases, a right-sided parietal lobe stroke leads to:
- Paresthesia, or abnormal sensations, on the left side of the body
- Weakness on the left side of the body
- Hemispatial neglect: a decreased awareness of the left side of the body and the environment on the left side
- Impaired spatial awareness of the environment on the left side of the body
- Difficulties with copying drawings
- Difficulties with sense of direction, and for visual and spatial memory
- Anosognosia: A lack of awareness of stroke symptoms, or that the stroke has even occurred
- In most cases, a left-sided parietal lobe stroke leads to:
- Paresthesia, weakness, hemispatial neglect, and/or impaired spatial awareness on the left side of the body
- Right-left confusion: difficulty with orientating the self to the left or right sides of one’s body or environment
- Agnosia: difficulties with recognising objects
- Acalculia: difficulty with counting
- Aphasia: speech and language issues; parietal lobe damage may also result in the inability to repeat others’ speech
- Agraphia: difficulty with writing
- An occipital lobe stroke happens when blood vessel blockage or bleeding prevents blood flow to the occipital lobes of the brain’s cerebral cortex.
- Occipital lobe strokes happen less often than strokes in the other cerebral lobes (temporal, parietal, and frontal lobes).
- Because the occipital lobes serve important functions in a person’s ability to perceive, process, and remember visual and spatial information, strokes that affect this brain area may strongly affect these abilities
- Occipital lobe stroke symptoms include:
- Vision loss:
- Heianopia: blindness on one side of the person’s field of vision
- A stroke that affects one side of the occipital lobe will affect the field of vision opposite to the affected brain area; for example damage to the left occipital lobe causes vision loss in the right half of the field of vision.
- Heianopia: blindness on one side of the person’s field of vision
-
-
- Quadrantanopia: blindness in one quadrant of the person’s field of vision
- Central vision loss: loss of sight in the centre (middle) of your field of vision
- Complete cortical blindness: Cortical blindness means total loss of sight due to damage in the brain’s cortex; this sight loss is not due to changes to the eyes.
- Anton syndrome: In some rare cases, persons with cortical blindness may be unaware that they are blind despite being shown evidence that that is the case
- Visual agnosia: an ability to recognise objects by sight
- Prosopagnosia, or face blindness: an ability to recognise the faces of people
- Word blindness: some people may be able to recognise letters and spell words, but not recognise words
- Visual hallucinations: though rare, persons may see images that do not originate from actual visual stimuli in their environment like sparks and lights
- Alexia without agraphia: an inability to read without difficulties with writing ability
- Difficulty with eye movement
- Nystagmus: Uncontrollable, constant, and rapid eye movements
- Control of eye movements: the nerves controlling the muscles that manage movements of different eye parts may be affected, which may cause eye misalignment and double vision, difficulties in tracking objects, difficulties with adapting to changes in light intensity, and eyelid drooping.
-
Tell us how we can improve?
- Health Promotion Board. (n.d.). Let’s talk about Vascular Dementia. HealthHub. https://www.healthhub.sg/programmes/mindsg/vascular-dementia
- Chiew, H. J. (2021, July 5). Young-onset dementia: Improving outcomes with early recognition at Primary Care. SingHealth. https://www.singhealth.com.sg/news/defining-med/Young-Onset-Dementia
- Ng, Z. X., Yang, W. R. E., Seet, E., Koh, K. M., Teo, K. J., Low, S. W., Chou, N., Yeo, T. T., & Venketasubramanian, N. (2015). Cerebellar strokes: A clinical outcome review of 79 cases. Singapore Medical Journal, 56(03), 145–149. https://doi.org/10.11622/smedj.2014195
- Ioannides K, Tadi P, Naqvi IA. Cerebellar Infarct. [Updated 2022 May 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470416/
- Huang, J., Qiu, Z., Zhou, P., Li, J., Chen, Y., Huang, R., Li, C., Ouyang, X., Feng, H., Xu, H., Liu, D., Dai, Z., Zhu, J., Liu, X., Chen, H., & Jiang, Y. (2019). Topographic location of unisolated pontine infarction. BMC Neurology, 19(1), 1-6. https://doi.org/10.1186/s12883-019-1411-6






